Electronic prescribing (e-prescribing) has transformed the way healthcare providers send prescriptions to pharmacies, reducing errors, improving patient safety, and speeding up the prescription process. However, its true potential is realized only when integrated seamlessly into an Electronic Health Record (EHR) system. Well-designed EHR integrations can make e-prescribing faster, more accurate, and more efficient for both providers and patients. Below are the top 10 EHR integrations that enhance the e-prescribing experience.
1. Drug Database Integration
An integrated drug database allows prescribers to search and select medications directly from a comprehensive, regularly updated list within the EHR. This reduces the risk of manual entry errors, ensures up-to-date drug information, and helps providers choose the right medication quickly. It also supports brand and generic drug options, dosage forms, and strengths, making the prescribing process more efficient.
2. Allergy and Adverse Reaction Alerts
Integrating allergy and adverse reaction data with e-prescribing is crucial for patient safety. The EHR can instantly flag any prescription that may cause allergic reactions or adverse drug interactions. These alerts help clinicians make informed decisions in real time, avoiding harmful outcomes and enhancing patient trust in the care process.
3. Drug Interaction Checks
When an EHR integrates drug-to-drug interaction checking, it automatically analyzes new prescriptions against a patient’s existing medication list. This ensures that harmful interactions are detected before the prescription is finalized, reducing hospital readmissions and improving patient outcomes. Such integration is especially important for patients managing multiple chronic conditions.
4. Prescription Drug Monitoring Program (PDMP) Access
A seamless PDMP integration within the EHR allows prescribers to check controlled substance histories without logging into a separate system. This saves time and ensures compliance with state regulations aimed at preventing opioid abuse and other prescription misuse. With one-click access, providers can make safer prescribing decisions while staying compliant with legal requirements.
5. Real-Time Prescription Benefit (RTPB) Integration
RTPB integration enables providers to see a patient’s medication costs and insurance coverage instantly during the prescribing process. This allows clinicians to select cost-effective options and prevent delays due to insurance rejections. By knowing the exact copay and coverage in real time, patients are more likely to fill their prescriptions promptly.
6. Electronic Prior Authorization (ePA)
Many medications require prior authorization from insurance companies before being dispensed. Integrating ePA into the EHR Software automates this process, allowing providers to submit and track authorizations electronically. This eliminates paperwork, speeds up approvals, and helps patients access necessary medications without unnecessary delays.
7. Pharmacy Directory Integration
An updated, searchable pharmacy directory within the EHR allows providers to send prescriptions directly to the patient’s preferred pharmacy. This integration includes address details, contact information, and even hours of operation, ensuring prescriptions reach the right location without confusion. It also facilitates same-day prescription filling for better patient adherence.
8. Medication History Retrieval
EHR systems that integrate medication history retrieval from insurance claims, pharmacies, and other healthcare providers give prescribers a complete picture of what a patient has been taking. This helps prevent duplicate prescriptions, improves coordination of care, and ensures the new prescription fits well into the patient’s treatment plan.
9. Clinical Decision Support (CDS) Tools
Integrating CDS tools within the EHR enhances e-prescribing by providing evidence-based recommendations, dosage calculators, and best-practice alerts. These tools assist providers in choosing the most effective treatment while avoiding common prescribing errors. With real-time guidance, clinicians can optimize patient care and improve overall prescribing accuracy.
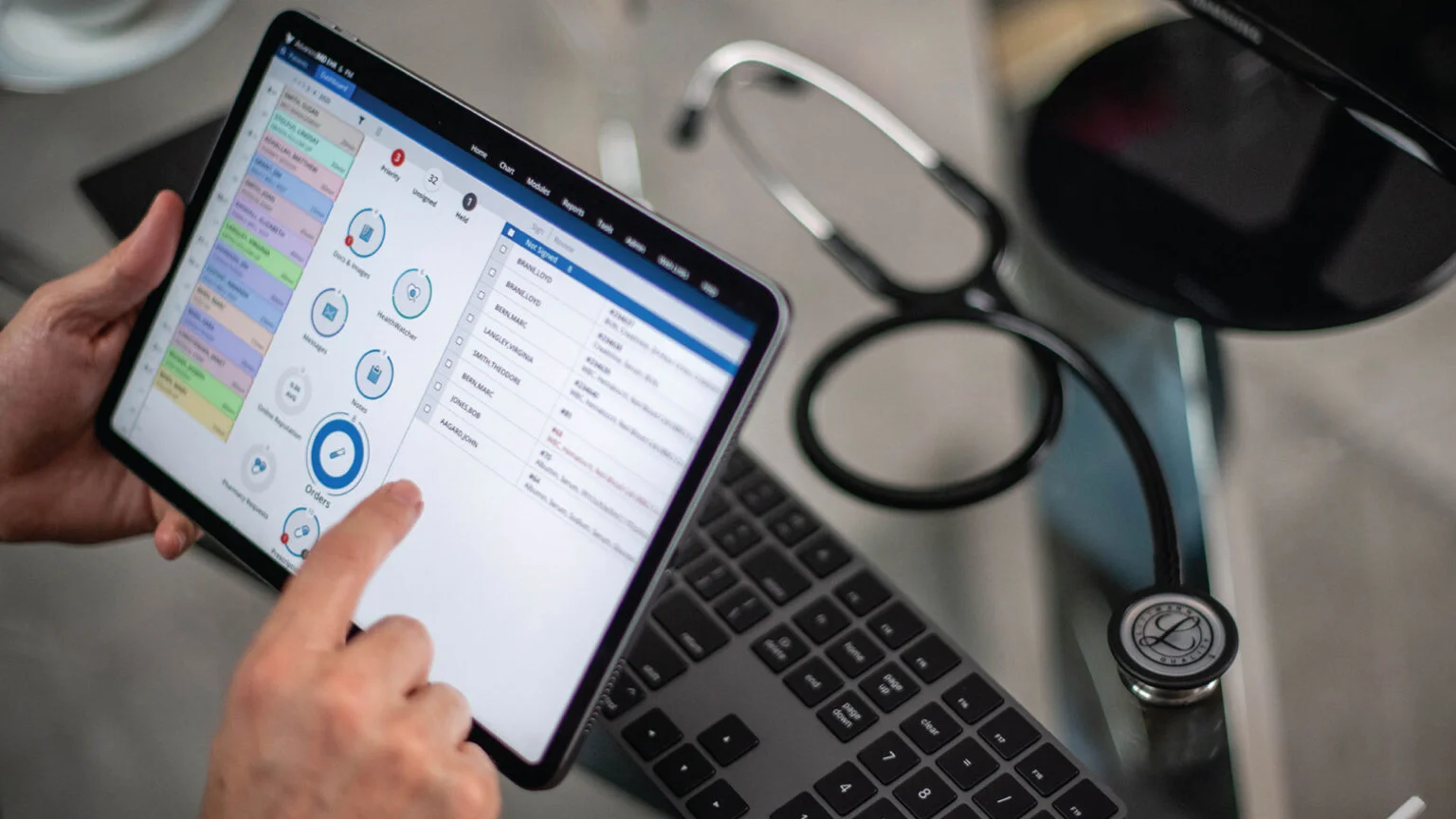
10. Mobile E-Prescribing Access
Modern EHR systems often integrate mobile access, enabling providers to send prescriptions securely from smartphones or tablets. This is especially useful for physicians working in multiple facilities or on-call situations. Mobile integration improves responsiveness and ensures patients receive their medications without delay, even outside traditional office hours.
Conclusion
E-Prescription Software has already proven to be a game-changer in healthcare, but when paired with the right EHR integrations, it becomes even more powerful. From drug databases and interaction checks to PDMP access and mobile prescribing, these integrations streamline workflows, reduce errors, improve compliance, and enhance patient satisfaction. For healthcare providers, adopting an EHR with strong e-prescribing integrations isn’t just about technology; it’s about delivering safer, faster, and more reliable patient care. As digital healthcare continues to evolve, these integrations will remain essential in building a more connected and efficient prescribing ecosystem.